The overall aim of our research is to understand the molecular mechanisms underlying the host-parasite interactions that lead to life-threatening malaria, and then use this knowledge to develop interventions to prevent or treat severe malaria.
1. Rosetting
Is there any potential for a PfEMP1-based vaccine to elicit antibodies to inhibit rosetting?
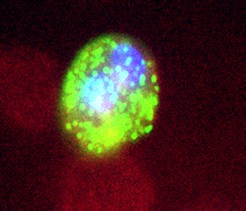
The ability of red blood cells infected with P. falciparum to bind uninfected red blood cells to form clumps of cells known as rosettes is associated with severe malaria (Rowe et al, 1995; Doumbo et al, 2009). The occurrence of rosettes in small blood vessels in the brain and other vital organs is thought to contribute directly to malaria pathogenesis by causing obstruction to blood flow which leads to hypoxia and tissue damage. Rosetting may also contribute to severe malaria by enhancing parasite growth and survival, leading to high parasitaemias in vivo (Rowe et al, 2002b). The importance of rosetting in severe malaria is indicated by the fact that naturally-occurring red blood cell polymorphisms that reduce rosetting, such as blood group O (Rowe et al 2007) or complement receptor 1 deficiency (Cockburn et al 2004) confer protection against severe, life-threatening malaria.
Previously we have defined the parasite ligand that mediates rosetting in one P. falciparum clone as a member of the variant surface antigen family PfEMP1, encoded by a specific var gene (Rowe et al, 1997; Claessens et al, 2011). We went on to show that rosetting in several different strains is mediated by a specific subset of PfEMP1 types called “group A” (Ghumra et al, 2012), which are associated with the most clinically severe malaria infections (Kyriacou et al, 2006; Kaestli et al, 2006). In addition, we identified human complement receptor one (CR1) as a receptor for rosetting on uninfected red blood cells (Rowe et al, 1997). We have subsequently localised the region of CR1 involved in rosetting, demonstrating that infected erythrocytes interact with the functionally important complement (C3b) binding site on CR1 (Rowe et al, 2000). This finding is important because it indicates that any treatment aimed at inhibiting the CR1 side of the rosetting interaction could impair normal CR1 functions such as phagocytosis and clearance of immune complexes, and could therefore be harmful.
Our current work is focussing on the parasite side of the rosetting interaction, studying the degree of variation in rosette-mediating var genes from different parasite isolates in order to determine the potential for a vaccine to elicit antibodies that would inhibit rosetting and prevent some cases of severe malaria. We have been able to produce PfEMP1 antigens as recombinant proteins in E. coli, and shown that we can immunize rabbits with these antigens to elicit potent antibodies that recognize the surface of infected erythrocytes, block rosetting and lead to opsonic phagocytosis of infected cells (Ghumra et al, 2011). Furthermore, the antibodies raised against PfEMP1 types from IgM-positive rosetting parasites are strain-transcending, and recognise heterologous parasite strains that show the same rosetting phenotype (Ghumra et al, 2012; Ghumra et al, in preparation). This suggests the existence of shared epitopes on rosette-mediating PfEMP1 types from different parasite strains that could be targeted in an anti-rosetting vaccine. We are also investigating naturally-acquired antibodies to rosetting PfEMP1 types in Kenyan children suffering severe malaria, in collaboration with Dr Pete Bull and Professor Kevin Marsh at the KEMRI/Wellcome Laboratories, Kilifi, Kenya.
What is the role of 'non-immune' IgM natural antibodies in rosetting?
We are also examining the role of serum factors such as IgM natural antibodies in rosetting (Rowe et al, 2002d), and have identified the IgM-binding domains of several PfEMP1 types implicated in rosetting (Ghumra et al, 2008; Ghumra et al, in preparation). In collaboration with Dr Richard Pleass, we have characterised the interaction between PfEMP1 and human IgM, and have shown that it is the Fc part of the IgM molecule that binds to infected erythrocytes (Ghumra et al, 2008; Czajkowsky et al, 2010).
Why do parasites rosette?
The biological function of rosetting is unknown, although it has been suggested that it may enhance erythrocyte invasion or promote immune evasion (reviewed in Rowe, 2005). We have recently investigated whether rosetting enhances parasite invasion of erythrocytes in the presence of host invasion-inhibitory antibodies to MSP-1. We found no evidence to support the hypothesis that rosetting enhances invasion (Deans and Rowe 2006b). We are currently investigating whether rosetting may be an immune evasion mechanism that helps the parasite avoid components of the host’s innate immune response such as NK cell activation or phagocytosis by monocytes or neutrophils (Corrigan and Rowe, 2010; Corrigan et al,). We are also interested in the host red cell receptors important for rosetting which may include Complement receptor 1, heparan sulphate-like molecules, Glycophorins and blood group antigens.
Can rosetting be reversed by drug treatment?
We have shown previously that rosettes can be disrupted by sulphated glycoconjugate drugs such as heparin (Rowe et al, 1994). Unfortunately, heparin is not recommended as a treatment for severe malaria because of its anti-coagulant side effects. We have recently shown that another sulphated glycoconjugate drug, curdlan sulfate, which has 10× lower anti-coagulant effect than heparin, inhibits rosetting in a wide range of P. falciparum isolates (Kyriacou et al, 2007) (work done in collaboration with Professor Ivan Havlik, University of Witwatersrand, South Africa). In collaboration with Dr Ed Yates and Dr Mark Skidmore at the University of Liverpool, we are investigating the possibility of developing rosette-disrupting carbohydrate compounds with no anti-coagulant side effects that could potentially be used as an adjunctive treatment for severe malaria (Skidmore et al, in preparation).
2. Human Brain Endothelial Cell (HBEC)-binding
What is the molecular basis of cytoadhesion to brain endothelial cells?
We have used an immortalized human brain endothelial cell line, HBEC-5i, as an in vitro model to study interactions between infected erythrocytes and HBEC cells underlying the development of cerebral malaria (Claessens and Rowe, 2012b). We examined the whole transcriptome of isogenic pairs of selected/unselected parasites and found that HBEC-selected parasites transcribe a specific subset of group A PfEMP1 types (different from those transcribed by rosetting parasites) (Claessens et al, 2012a). This PfEMP1 subset is a potential target for adjunctive therapies to treat cerebral malaria, currently the most deadly of all malaria complications. We are currently investigating diversity in HBEC-binding PfEMP1 types, and the possibility of raising strain-transcending antibodies against HBEC-binding infected erythrocytes.
3. Platelet-mediated clumping
What is the molecular basis of platelet-mediated clumping?
Platelet-mediated clumping of infected erythrocytes is a parasite adhesion phenotype that is distinct from rosetting and has previously been associated with severe malaria in different parts of the world (Kenya: Pain et al, PNAS 2001, Thailand: Chotivanich et al, J Infect Dis 2004). However, in a recent study in Mali we found that clumping was primarily associated with high parasitaemia rather than severe clinical symptoms (Arman et al, 2007). We have also discovered that the in vitro assay for clumping is highly influenced by the precise conditions used (haematocrit, parasitaemia and pH all greatly influence the outcome of the assay) (Arman and Rowe, 2008; Arman et al, 2013). We suggest that previous disease-association studies may not have been done under optimal conditions, therefore the association between clumping and severe malaria requires further investigation. The molecular basis of clumping is currently unclear, although human platelet CD36 is known to be essential. We are currently investigating the role of var genes/PfEMP1 as parasite ligands for clumping, and examining the role of various platelet molecules as clumping receptors. We developed a method to allow selection of clumping-positive and clumping negative isogenic pairs of parasites (Arman et al, 2013), and we have examined the transcriptomes of selected parasites to look for genes whose expression is increased after selection for clumping (Arman et al, in preparation).
4. Complement receptor one (CR1)
How do CR1 polymorphisms affect susceptibility to severe malaria?
Identification of CR1 as a rosetting receptor on uninfected red blood cells (Rowe et al, 1997) was of particular interest because several polymorphisms of the CR1 gene occur at high frequency in malarious countries but are rare in non-malarious regions (reviewed in Rowe et al, 2009b). We hypothesised that these CR1 polymorphisms may have been selected to high frequency because they reduce the ability of P. falciparum parasites to form rosettes and thereby protect against severe malaria. We discovered that in Papua New Guinea, a human CR1 polymorphism that causes red blood cell CR1 deficiency is extremely common and does confer significant resistance to severe malaria, reducing the odds ratio for severe disease by about two thirds (Cockburn et al, 2004). CR1 deficiency appears to be common in Asia and Oceania, but is rare in Africa. However, several CR1 polymorphisms that cause single amino acid changes in the LHR-D portion of CR1 occur at high frequency in African populations (Moulds et al 2001). We have investigated whether the African CR1 polymorphisms influence susceptibility to severe malaria in Kenya (collaboration with Prof Tom Williams, KEMRI-Wellcome laboratories, Kilifi, Kenya) and Mali (collaboration with Professor Ogo Doumbo, Malaria Research and Training Centre, Bamako, Mali, Professor Chris Plowe and Dr Kirsten Lyke, University of Maryland, USA and Dr Joann Moulds, LifeShare Blood Centers, Louisana, USA). This work has uncovered a complex but fascinating effect of CR1 polymorphisms on susceptibility to multiple diseases (Opi et al, in preparation). We are also investigating the structural and functional effects of CR1 polymorphisms (Tetteh-Quarcoo et al, 2012; Opi et al, in preparation).